What is Palliative Care for Lung Cancer?
Palliative care, or supportive care, is a medical specialty that is focused on symptom management rather than curative effects. This type of care can provide the medical, emotional, and practical support you may need when faced with a diagnosis like cancer. Palliative care is not the same as hospice or end-of-life care and can be utilized at any point post-diagnosis (insurance permitting), while also receiving treatment for your cancer. It’s designed to prioritize quality of life while remaining committed to treatment needs.
When you’re going through treatment for non-small cell lung cancer (NSCLC), your body- as well as your mind- will likely face some unfamiliar side effects. While your care team is always there to offer you support, palliative care is another resource you can utilize to help ease the symptoms you’re experiencing.
No matter your treatment path – chemotherapy, radiation, surgery – you’re likely to feel its toll on your body. Common symptoms can include pain, fatigue, nausea, depression, anxiety, and shortness of breath, among others.
The struggle can often be beyond what you expected, so make sure you’re proactive about understanding both the emotional and physical benefits of palliative care and when and where to receive treatment.
Evidence-based guidance powered by NCCN Guidelines®
Personalized treatment plans shaped by the latest oncology standards—tailored to your diagnosis.
Get started
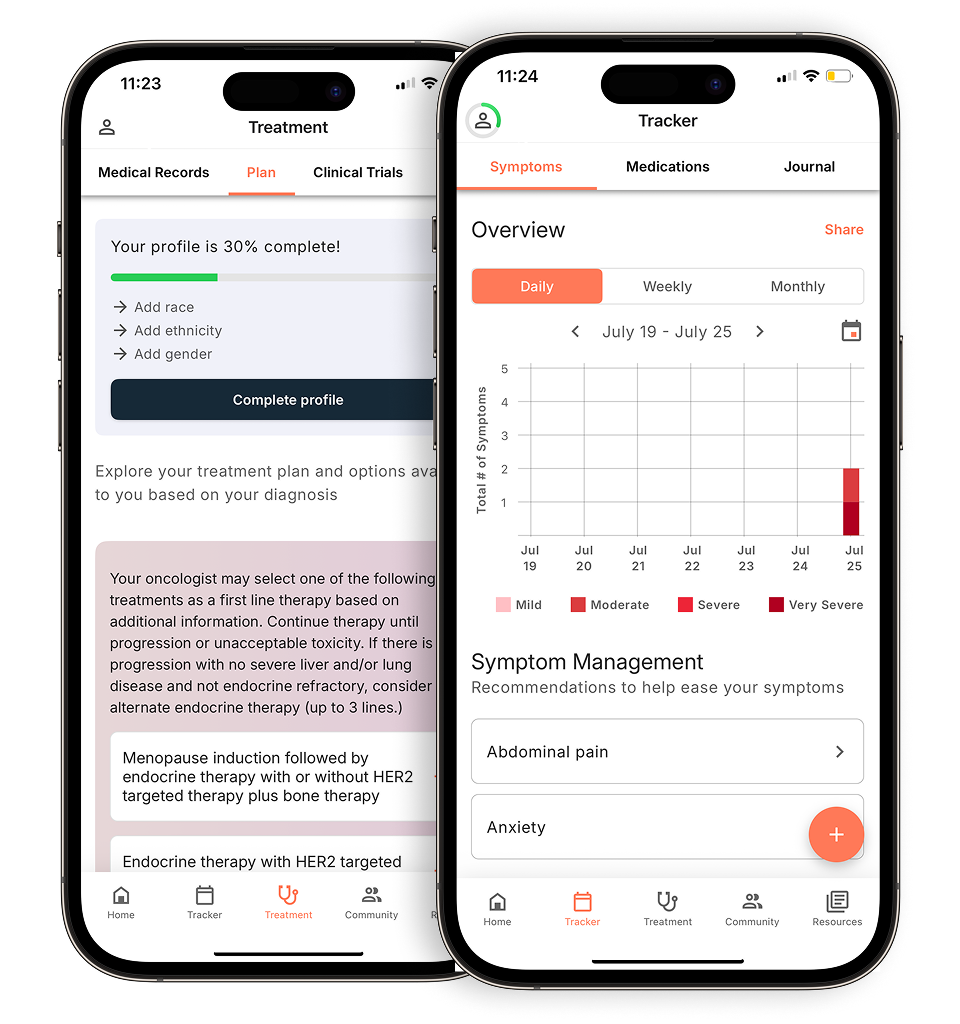
View your personalized treatment plan in the Outcomes4Me app
Use your diagnosis to unlock personalized NCCN Guidelines®-aligned recommendations.
Continue in app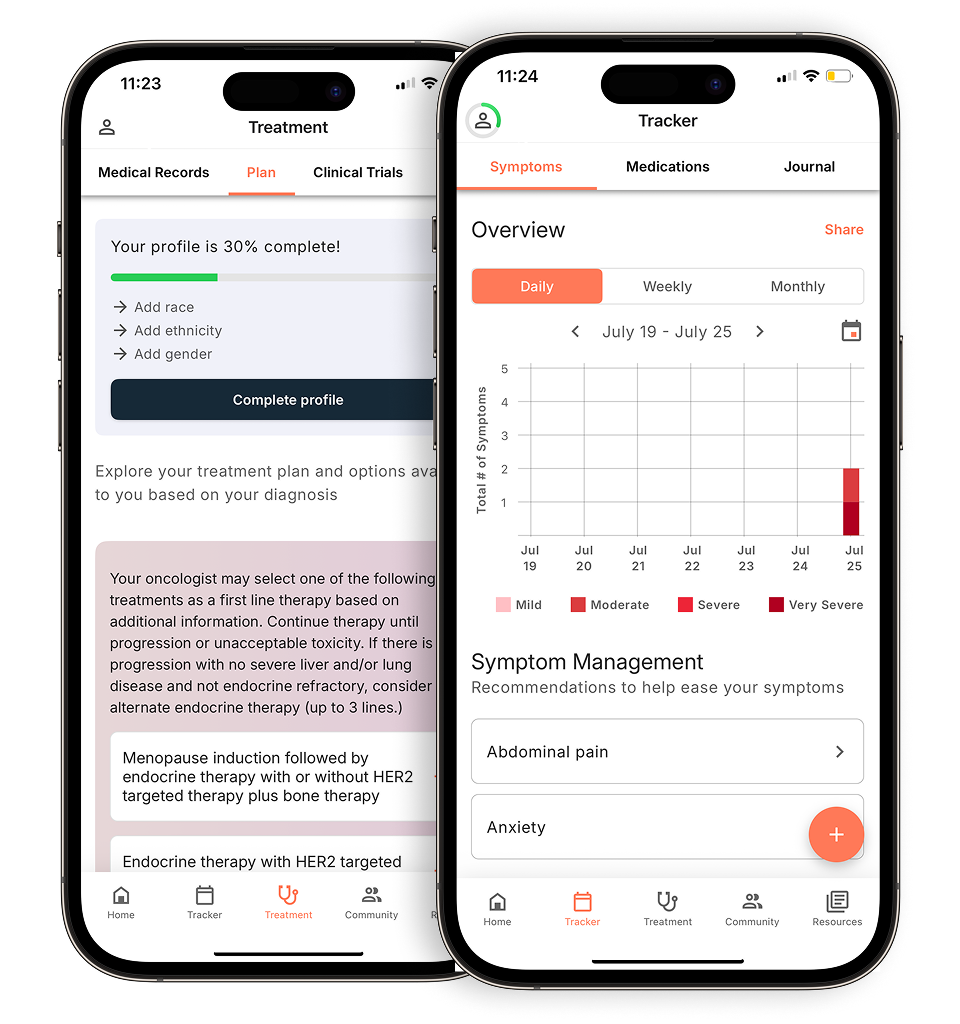
1. You’re in a lot of pain
With NSCLC, you might experience coughing and pain throughout treatment. A palliative care team can work directly with your oncologist and prescribe medication if that makes sense as a recommended therapy for your pain. Pain medicine options include NSAIDs, opioids, antidepressants, and steroids.
Palliative care is meant to help you feel more comfortable through your diagnosis and treatment, so don’t feel like your pain isn’t “bad enough” to seek medication or help. If you’re not sure when to ask for additional support, the American Lung Association offers a worksheet that helps you navigate why and when to ask for palliative care. Palliative care is meant to help you feel more comfortable through your diagnosis and treatment, so don’t feel like your pain isn’t “bad enough” to seek medication or help. If you’re not sure when to ask for additional support, the American Lung Association offers a worksheet that helps you navigate why and when to ask for palliative care. You can also use a chemotherapy side effect tracker, such as the symptom tracker in the Outcomes4Me app, to monitor changes in how you’re feeling so your care team can evaluate whether palliative care may be helpful.
2. You’re having trouble breathing
If fluid builds up in your chest outside your lungs, it can push on your lungs and make it difficult for you to breathe. This symptom, called a pleural effusion, can be treated through a few palliative care procedures designed to drain or remove the fluid and make breathing easier including thoracentesis, pleurodesis, or catheter placement.
If your cancer has grown into an airway in your lung, you might find yourself short of breath. In this case, your care specialist might recommend radiation therapy, photodynamic therapy for early-stage tumors, laser therapy for smaller tumors, or stent placement when other therapies don’t work. Medications and oxygen therapy can also help you breathe better.
3. You’re depressed or feeling anxious
A therapist can provide you with cognitive exercises to monitor your symptoms and tools to help you navigate through the emotional pain. From meditation to yoga, daily walks to gratitude journals, there are several ways available to get the help you need.
A palliative care expert can also provide a safe space to talk and medicine to help combat your depression and anxiety.
4. You can’t eat
If you’re going through treatment, chances are you might experience nausea, loss of appetite, vomiting, or constipation. Through palliative care, a nutritionist can help you better manage your diet, find foods to eat that feel a little better going down, and monitor your nutritional and caloric intake.
5. You’d be open to alternative approaches
Your oncology and palliative care teams might recommend physical therapy or yoga to help with the pain. For more chronic pain and stress relief, ask your specialist about complementary therapies for the mind and body, such as massage, guided imagery, or acupuncture.
If you and your family have more questions about the benefits of palliative care, the American Cancer Society offers a list of questions to ask your oncology team. Palliative care can take place at a hospital, outpatient clinic, treatment center or right at home. Many types of palliative care may be covered by private health insurance, Medicare, or Medicaid.
If you have additional questions about palliative support care or you’d like to speak with someone, you can connect with an Outcomes4Me oncology nurse practitioner at no charge through the Outcomes4Me app, using the “Ask Outcomes4Me” button.
Personalized support for real care decisions
Understand your diagnosis, explore clinical trials, and track symptoms--all in one place.
Get started
Compare treatments, prepare for appointments, and track side effects—all in the app
Built for your diagnosis, Outcomes4Me gives you the tools to make confident, informed decisions—right when you need them.
Continue in app