Last week top breast cancer oncologists and researchers attended the 43rd Annual San Antonio Breast Cancer Symposium (SABCS), the premier conference for presenting the latest breast cancer data to an international audience. The conference features breakthrough clinical trial results, promising novel approaches to treatment and solutions to current gaps in clinical care. We’ve highlighted a few major takeaways from the conference.
Research in early-stage breast cancer
Many of this year’s presentations focused on how to optimize early-stage treatment and effectively prevent recurrence in high-risk patients. Researchers have begun to evaluate the benefit of CDK4/6 inhibitors in early-stage high-risk breast cancer. Updated results from the phase III MONARCH E trial showed HR+/HER2- high risk patients who received abemaciclib with endocrine therapy had a 29% reduced risk of recurrence after two years compared to endocrine therapy alone1. The PENELOPE-B trial, studying the use of another CDK4/6 inhibitor, palbociclib, with endocrine therapy in early-stage HR+/HER2- breast cancer, found that adding palbociclib to adjuvant therapy showed no increased benefit in invasive-disease free survival2. Researchers will need to monitor follow up of the MONARCH E trial to see if there is a sustained long-term benefit to adding abemaciclib to endocrine therapy for HR+/HER2- high risk breast cancer patients.
Neratinib was recently approved for HER2+ metastatic breast cancer and researchers are now studying neratinib in early-stage breast cancer. Overall survival results from the phase III EXTENET trial show that HR+ breast cancer patients who started neratinib within one year of completing adjuvant trastuzumab and who did not achieve a pathologic complete response after neoadjuvant trastuzumab had an increase of 9.1% in overall survival at eight years compared to the placebo group3. Additionally, HR+ patients taking neratinib after adjuvant trastuzumab had fewer incidents of central nervous system metastases compared to the placebo group.
It is also important to know when additional treatment, and related side effects, are not necessary. The Oncotype DX Recurrence Score is commonly used to determine if HR+/HER2-, lymph node negative breast cancer patients can safely forego adjuvant chemotherapy. However, this does not apply to patients with lymph node positive breast cancer as patients with node positive cancer have a higher risk of recurrence. The RXPONDER study found that HR+/HER2- postmenopausal breast cancer patients with a Recurrence Score below 25 did not see an increased benefit from adjuvant chemotherapy and can likely forego adjuvant chemotherapy4. However, premenopausal women showed significant benefit from adjuvant chemotherapy and should consider combined endocrine therapy and chemotherapy. Further studies are needed to understand quality of life implications and other outcomes.
Research in metastatic breast cancer
Data presented in the metastatic setting included promising results of new therapies and confirmation of benefit in already approved therapies. Currently, a CDK4/6 inhibitor in combination with endocrine therapy is the standard of care for HR+/HER2- metastatic breast cancer. Updated overall survival results from the phase III MONALEESA-7 trial confirmed the benefit of adding ribociclib to endocrine therapy in pre-menopausal patients with HR+/HER2- metastatic breast cancer5. Patients taking ribociclib and endocrine therapy had a median overall survival of 58.7 months, the longest reported overall survival in HR+/HER2- metastatic breast cancer, compared to 48 months in patients on endocrine therapy alone. The addition of ribociclib also significantly lengthened the time till chemotherapy. These data are continued evidence that ribociclib with endocrine therapy should be considered for pre-menopausal HR+/HER2- metastatic breast cancer.
Much of the research in the metastatic setting focused on triple negative breast cancer (TNBC), a relatively more aggressive cancer subtype. Updated results from the phase III KEYNOTE trial demonstrated pembrolizumab’s clinical benefit in metastatic TNBC patients with PD-L1 expressing tumors6. PD-L1 positive, TNBC patients receiving immunotherapy, pembrolizumab, with chemotherapy experienced an increased median progression free survival of 4.1 months compared to patients taking chemotherapy alone. These results support the addition of pembrolizumab to standard chemotherapy in first-line treatment of metastatic TNBC. Based on these results, pembrolizumab was granted accelerated approval by the FDA for patients with metastatic TNBC with PD-L1 expressing tumors.
Another novel therapy presented at SABCS was enobosarm, a selective androgen receptor targeting agent. In a phase II trial, enobosarm showed clinical benefit in 32% of in ER+/HER2- metastatic breast cancer patients who are resistant to endocrine therapy and chemotherapy7. Enobosarm was well tolerated and women reported improvements in quality of life measures like mobility, anxiety and pain discomfort. Enobosarm was approved for a phase III trial, to evaluate the efficacy and safety of enobosarm in previously treated ER+/HER2- metastatic breast cancer.
Disparities in breast cancer care
Discussions at SABCS also focused on inequities in breast cancer care. Currently, women of color with breast cancer have worse survival outcomes compared to white women. Dr. Olufunmilayo Olopade presented data showing that overall black women have higher mortality rates and an 8.5% lower pathological complete response rate to treatment8. Presenters ask why this is and, more importantly, what we can do to change this.
Presenter, Dr. Lisa Newman, says, “most genome association studies today have been lacking in population diversity, particularly with regard to African ancestry”9. By collecting data on more diverse populations and using AI, Dr. Olopade, says we will be able to effectively personalize treatment based on actionable germline and somatic mutations, not just disease subtypes, demographics or insurance. This genetic information and the inclusion of more women of color in clinical trials will allow scientists to improve personalized cancer care to underserved populations. According to Dr. Olopade, we are only at the tip of the iceberg when it comes to personalized medicine.
Patient engagement and education
Research shared at SABCS showed there is a critical need to improve breast cancer patient education tools. Multiple studies reported a lack of awareness of biomarker testing among breast cancer patients. One study showed only 22% of patients were familiar with or aware of biomarker testing, but 75% of participants were very likely or likely to ask their provider about testing if it could impact their treatment10. Outcomes4me presented a study showing only 27% of metastatic patients received genomic testing and 41% of participants were unaware of genomic testing11. These studies show breast cancer patients are not receiving the information they need to make informed treatment decisions. Improved methods of patient engagement and education are needed.
Symptom management to improve breast cancer care
Patient-reported outcomes (PROs) are increasingly being used in clinical trials and symptom management. There have been multiple studies presented at SABCS focusing on the use of PROs. One study found that the use of a web-based symptom management tool helps patients normalize symptoms, increases awareness of symptoms and complements the information given to them by their doctor12. In this study 90% of patients reported sexual health side effects and 87% reported anxiety and stress, symptoms which are not always captured in health records. An additional study utilized PROs to better understand the psychosocial distress in young breast cancer patients. 52% of patients reported decreased well being and 44% reported elevated anxiety13. However, the referral rates to psychosocial oncology or survivor clinics was lower, 24%-36%, showing a clear gap in addressing the psychological needs of patients.
References:
- O’Shaughnessy, Joyce, et al. Primary outcome analysis of invasive disease-free survival for monarchE: abemaciclib combined with adjuvant endocrine therapy for high risk early breast cancer. Presented at: 2020 Virtual San Antonio Breast Cancer Symposium; December 8-11, 2020. Abstract GS1-01.
- Loibl, Sibylle, et al. Phase III study of palbociclib combined with endocrine therapy (ET) in patients with hormone-receptor-positive (HR+), HER2-negative primary breast cancer and with high relapse risk after neoadjuvant chemotherapy (NACT): First results from PENELOPE-B. Presented at: 2020 Virtual San Antonio Breast Cancer Symposium; December 8-11, 2020. Abstract GS1-02.
- Holmes, Frankie Ann, et al. Continued efficacy of neratinib in patients with HER2-positive early-stage breast cancer: Final overall survival analysis from the randomized phase 3 ExteNET trial. Presented at: 2020 Virtual San Antonio Breast Cancer Symposium; December 8-11, 2020. Abstract PD3-03.
- Kalinsky, Kevin, et al. First results from a phase III randomized clinical trial of standard adjuvant endocrine therapy (ET) +/- chemotherapy (CT) in patients (pts) with 1-3 positive nodes, hormone receptor-positive (HR+) and HER2-negative (HER2-) breast cancer (BC) with recurrence score (RS) < 25: SWOG S1007 (RxPonder). Presented at: 2020 Virtual San Antonio Breast Cancer Symposium; December 8-11, 2020. Abstract GS3-00.
- Tripathy, Debu, et al. Updated overall survival (OS) results from the phase III MONALEESA-7 trial of pre- or perimenopausal patients with hormone receptor positive/human epidermal growth factor receptor 2 negative (HR+/HER2−) advanced breast cancer (ABC) treated with endocrine therapy (ET) ± ribociclib. Presented at: 2020 Virtual San Antonio Breast Cancer Symposium; December 8-11, 2020. Abstract PD2-04.
- Rugo, Hope, et al. Additional efficacy endpoints from the phase 3 KEYNOTE-355 study of pembrolizumab plus chemotherapy vs placebo plus chemotherapy as first-line therapy for locally recurrent inoperable or metastatic triple-negative breast cancer. Presented at: 2020 Virtual San Antonio Breast Cancer Symposium; December 8-11, 2020. Abstract GS3-01.
- Palmieri, Carlo, et al. Efficacy and safety of enobosarm, a selective androgen receptor modulator, to target AR in women with advanced ER+/AR+ breast cancer – final results from an international Phase 2 randomized study. Presented at: 2020 Virtual San Antonio Breast Cancer Symposium; December 8-11, 2020. Abstract PD8-10.
- Olopade, Olufunmilayo , et al. Not a One Size Fits All: Personalized Medicine for the Underserved. Presented at: 2020 Virtual San Antonio Breast Cancer Symposium; December 8-11, 2020. Special Session 1.
- Newman, Lisa. Socioeconomic Access Matters. Presented at: 2020 Virtual San Antonio Breast Cancer Symposium; December 8-11, 2020. Special Session 1.
- Rugo, Hope, et al. Patient knowledge, attitudes and perceptions regarding breast cancer biomarkers, testing, and quality of life. Presented at: 2020 Virtual San Antonio Breast Cancer Symposium; December 8-11, 2020. Abstract PS9-28.
- Stroiney, Amanda, et al. Understanding genomic testing in real-world populations at outcomes4Me (GENOME). Presented at: 2020 Virtual San Antonio Breast Cancer Symposium; December 8-11, 2020. Abstract PS9-42.
- Sella, Tal, et al. Young, empowered & strong (YES): A web-based education and supportive care intervention for young women with breast cancer across the care continuum. Presented at: 2020 Virtual San Antonio Breast Cancer Symposium; December 8-11, 2020. Abstract P12-08.
- Krishnamurthy, Revathy, et al. Patient-reported outcomes of adolescents and young adults with breast cancer treated with curative intent. Presented at: 2020 Virtual San Antonio Breast Cancer Symposium; December 8-11, 2020. Abstract P12-09.
Personalized support for real care decisions
Understand your diagnosis, explore clinical trials, and track symptoms--all in one place.
Get started
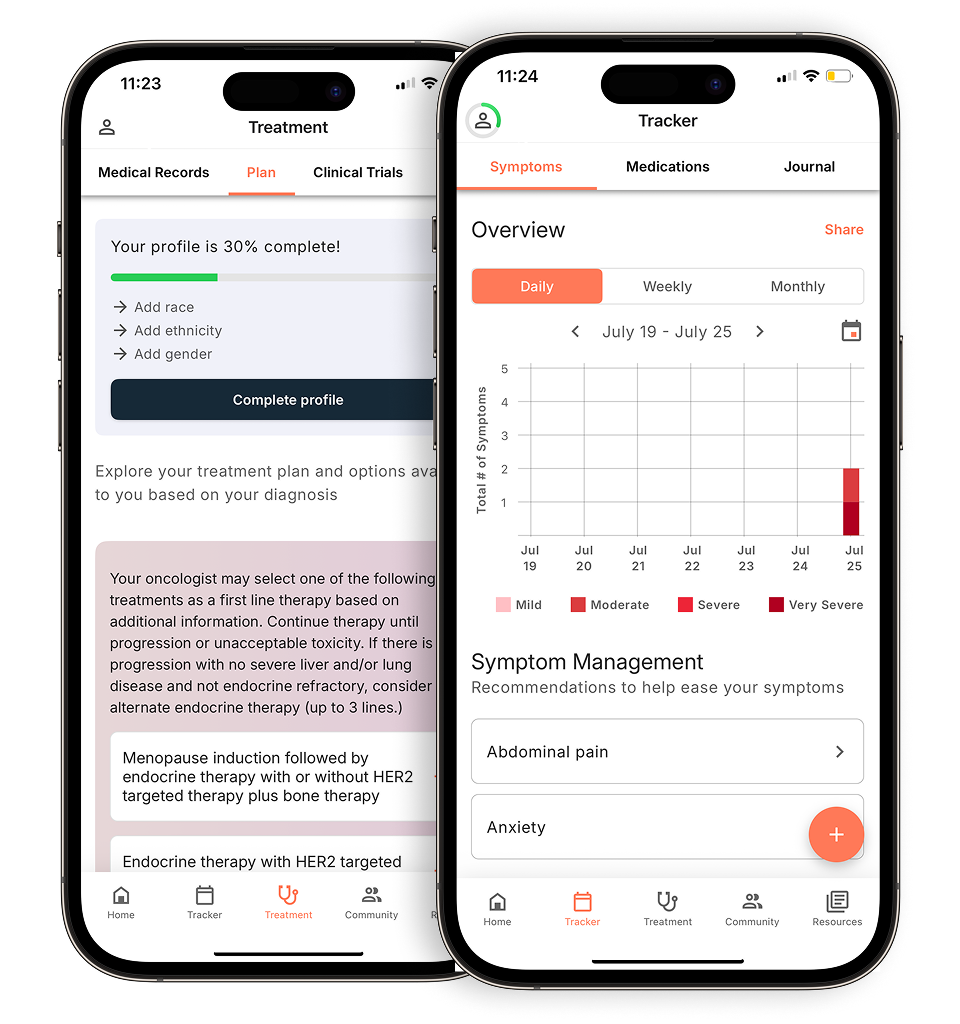
Compare treatments, prepare for appointments, and track side effects—all in the app
Built for your diagnosis, Outcomes4Me gives you the tools to make confident, informed decisions—right when you need them.
Continue in app