For Lung Cancer Awareness Month, we were fortunate to host Palomar Health’s Dr. Hardeep Phull for our Ask the Expert webinar. Dr. Phull covered a variety of topics and provided a comprehensive breakdown of non-small cell lung cancer (NSCLC). You can watch the full webinar, below.
We’ve also transcribed some of the highlights and questions surrounding an initial NSCLC diagnosis from the discussion.
The following questions and responses have been lightly edited for grammatical purposes.
Q: What are the symptoms of lung cancer to look out for?
A: There are many types of lung cancer. There’s small cell, non-small cell, and some other neuroendocrine and nonspecific types. Non-small cell lung cancer is the most common.
Believe it or not, some of these have no symptoms and sometimes it’s very insidious. What I mean by that is we have a lot of patients that go in for something like an X-ray for an employment physical or they’re in the ER and they find something.
Unfortunately, we incidentally find way too many cancers like that. Lung cancer, if you think of it as a lung nodule, could start less than an inch. It could be barely noticeable even on a CT scan and not all of us are getting X-rays and CT scans every year.
In the advanced stages, lung cancer can cause coughing and shortness of breath. If there’s fluid in the lungs, even if it’s close to the airways, it could cause coughing up of blood. One of the first things I tell my patients though, is that COVID, pneumonia, or any viral infection can mimic the symptoms of lung cancer.
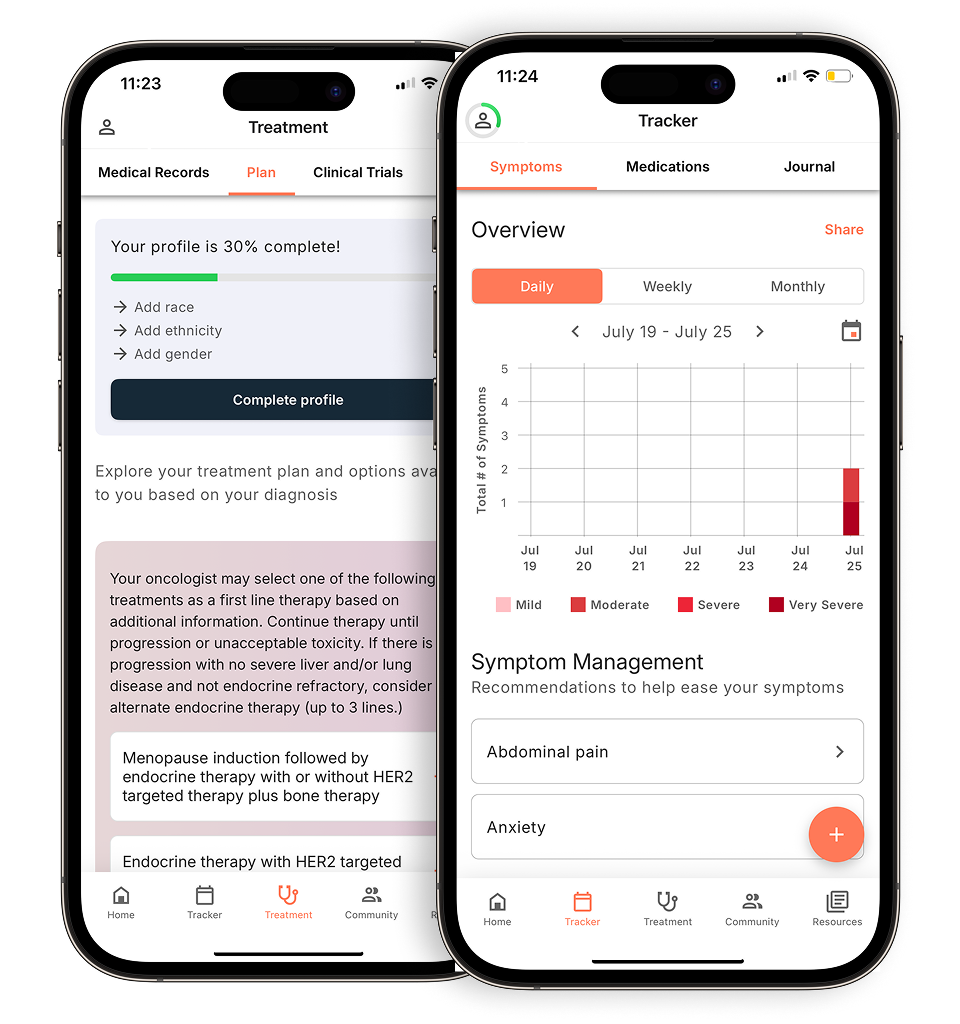
Evidence-based guidance powered by NCCN Guidelines®
Personalized treatment plans shaped by the latest oncology standards—tailored to your diagnosis.
Get started
View your personalized treatment plan in the Outcomes4Me app
Use your diagnosis to unlock personalized NCCN Guidelines®-aligned recommendations.
Continue in app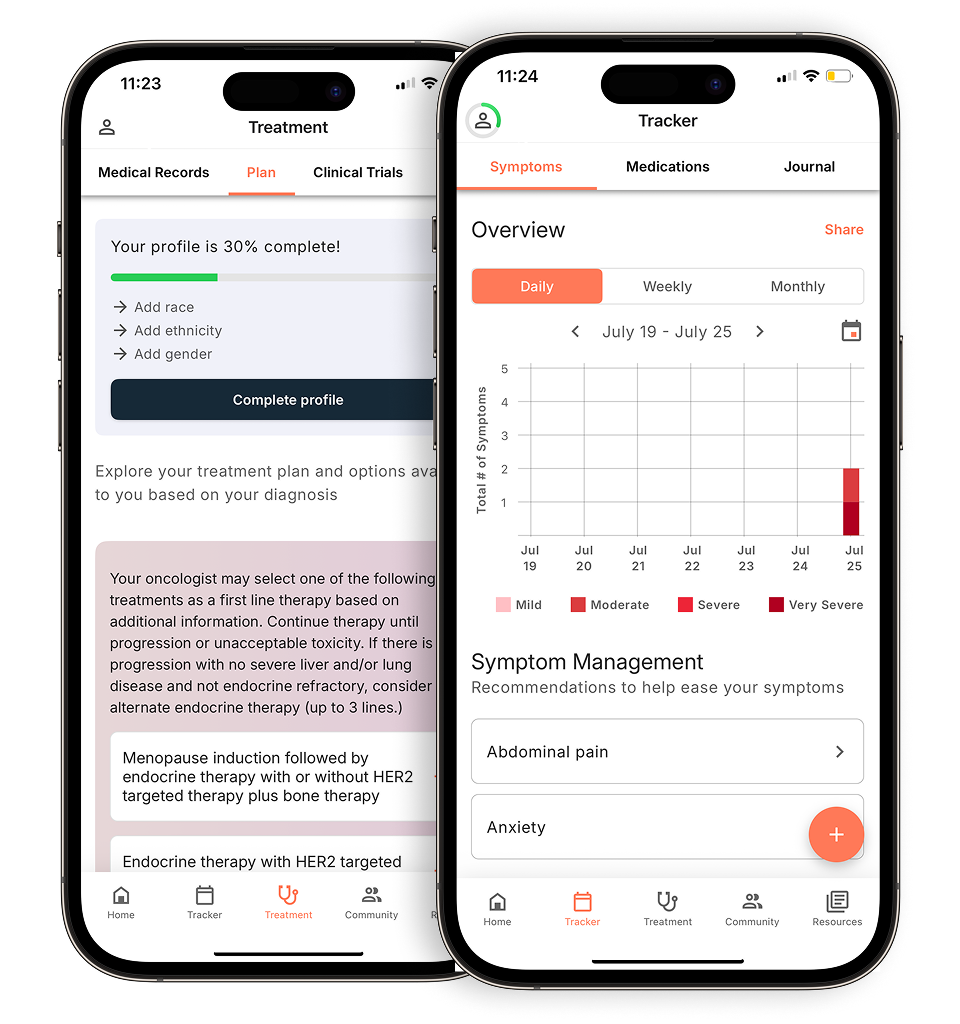
If it spreads to other parts of the body like the bone or even the brain, which is a common metastatic site, you could have pain in those areas. You could have headaches or even memory changes. Those are very advanced stages.
The other thing is people who exercise. One of the best things about exercise and being active is you know your normal. If you can’t achieve that anymore, you can say “Something is wrong with me. This isn’t my norm, I’m really fatigued.”
Again, these are nonspecific things, but the more someone knows their baseline, the more they know something is off. Antibiotics didn’t work, inhalers aren’t doing anything, and things are feeling progressively off. That’s when you dig a little deeper
Q: What treatments are available for smokers who have lung cancer? Are non-smokers at risk of lung cancer?
A: I wrote an article recently with a colleague of mine called The Cancer Blame Game. What we meant by that was in many cultures and just in general, it’s very easy to blame patients or their smoking as to why they got lung cancer. Other things like diet, exercise, and alcohol use can play a part too. Yes, we have control over our lives and what we can and cannot do, but I’ll be honest, not every lung cancer is a smoking-related lung cancer.
In fact, we find many of the adenocarcinomas, which is a type of non-small cell lung cancer, are non-smoking associated. These have some of the most exciting genetic mutations. I say exciting because that field has taken off. What started as maybe having a couple of mutations called EGFR and ALK and developing drugs for those. We used to have just one or two drugs for each, but now it has blossomed into a field where you have several known mutations in those classes and a dozen others which we now call oncolytics.
Not everything is a smoking-associated cancer. Of course, we have smokers who have lung cancer. Those are typically squamous cell cancers, but even for those cases I have seen certain interesting genetic profiles. What’s interesting is smokers often will upregulate PDL1, which is a checkpoint inhibitor marker.
Everyone’s heard of immunotherapy. What’s interesting is that some of those patients do well on immunotherapy because their lung tissues are so mutated, maybe from smoking, that they often express these additional biomarkers and the cells are super mutated. They’re always being surveyed by the immune system.
But that’s actually to the benefit of the patient in some cases. So I’m not saying go and smoke, you’ll do better with immunotherapy; what I’m saying is not everyone with lung cancer is a smoker. If you are, there’s still hope and there are still treatments that could be targeted. Many patients are non-smokers and you can get lung cancer without a single exposure to a cigarette.
When I meet a patient, we ask if they smoke, but it’s not a judgmental question. It’s more to get to the root of the symptoms and the options I have for this person.
Q: Who’s on a lung cancer care team?
A: I call it the trifecta of oncological care, but it’s actually more than a trifecta now. Usually, an oncologist, like me, does the chemotherapy or the oncolytics. Sometimes, there’s a radiation doctor involved, especially for early-stage cancers. That’s a radiation oncologist. There’s a surgeon. If this is an early resectable cancer, it’s very important to have a good thoracic surgeon, or we call it a CT surgeon, cardiothoracic or thoracic.
In my opinion, the most important part is pulmonology. They often drive the quarterback, especially when it comes to diagnostics and deciding what order we do things.
Most big institutions have a tumor board and they discuss these cases together. We have all these people in the room to provide their opinions and discuss things like surgery and in what order.
It’s a team-based approach where not one person is right or wrong but rather, what is best for this individual in front of us? What do we all think and what should we do first?
That is the best evidence-based way to practice, even though it sounds like you’re just having a pow-wow about the patient in private. How is that possibly evidence-based?
It’s a very systematic way to discuss patients’ cases and bring up all the nuances. Radiologists and pathologists are also at these meetings. Radiologists are doctors who look at images and pathologists are doctors who take the biopsy, classify it, and get the diagnosis.
All of these people on the team are important. No one can do it without everyone, so you have a very powerful team when you put them in a room together. They can make good decisions for these patients, especially for the more complicated cases.
To view the entirety of Dr. Phull’s Ask the Expert webinar, click here.
Personalized support for real care decisions
Understand your diagnosis, explore clinical trials, and track symptoms--all in one place.
Get started
Compare treatments, prepare for appointments, and track side effects—all in the app
Built for your diagnosis, Outcomes4Me gives you the tools to make confident, informed decisions—right when you need them.
Continue in app