We recently hosted Dr. Martin F. Dietrich, a medical oncologist at the Cancer Care Centers of Brevard and an assistant professor of internal medicine at the University of Central Florida, for a recent Outcomes4Me “Ask the Expert” webinar.
You can watch Dr. Dietrich’s full webinar, below.
We’ve transcribed some of the key discussion points from the webinar. If you or a loved one have been recently diagnosed with non-small cell lung cancer (NSCLC), we hope you’ll find Dr. Dietrich’s perspective informative.
You can read part one of our Dr. Dietrich webinar recap, which examines NSCLC staging and testing options, here.
The following questions and responses have been lightly edited for grammatical purposes.
Q: If there isn’t enough tissue available for testing what are what are patients’ options?
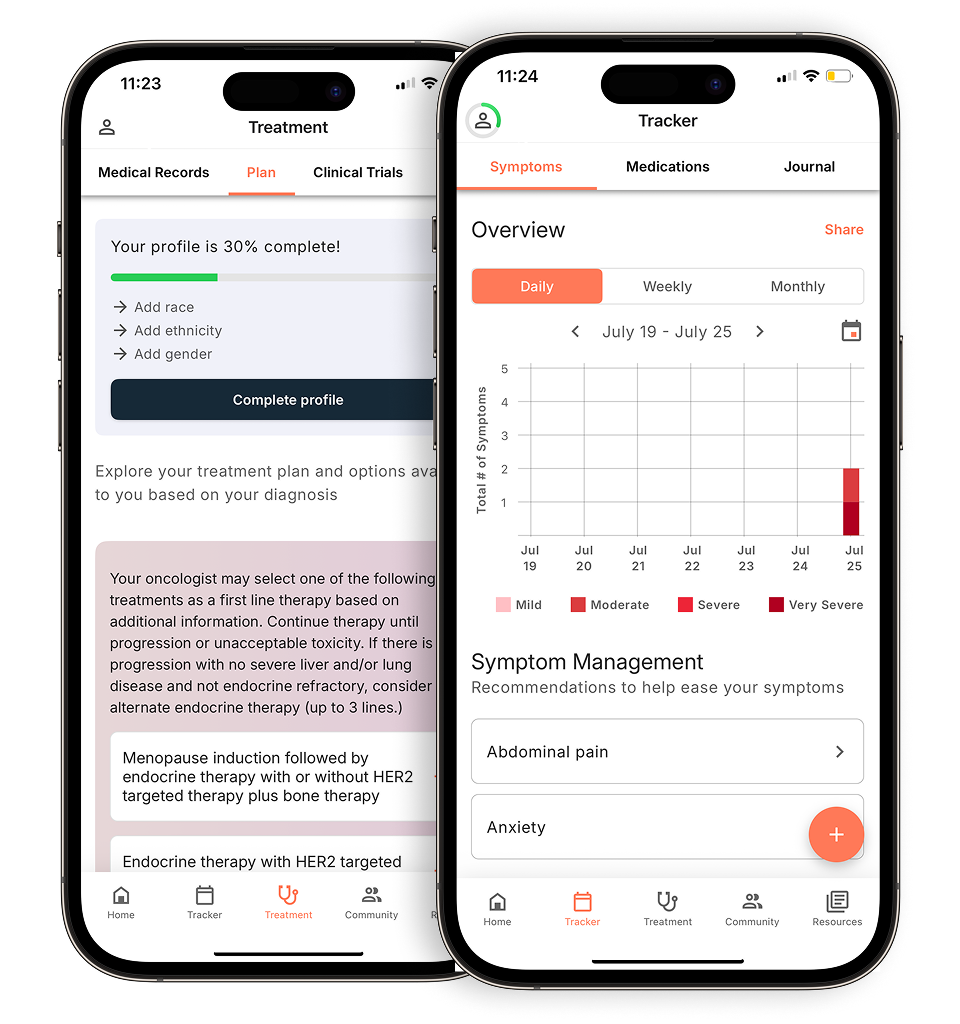
Evidence-based guidance powered by NCCN Guidelines®
Personalized treatment plans shaped by the latest oncology standards—tailored to your diagnosis.
Get started
View your personalized treatment plan in the Outcomes4Me app
Use your diagnosis to unlock personalized NCCN Guidelines®-aligned recommendations.
Continue in app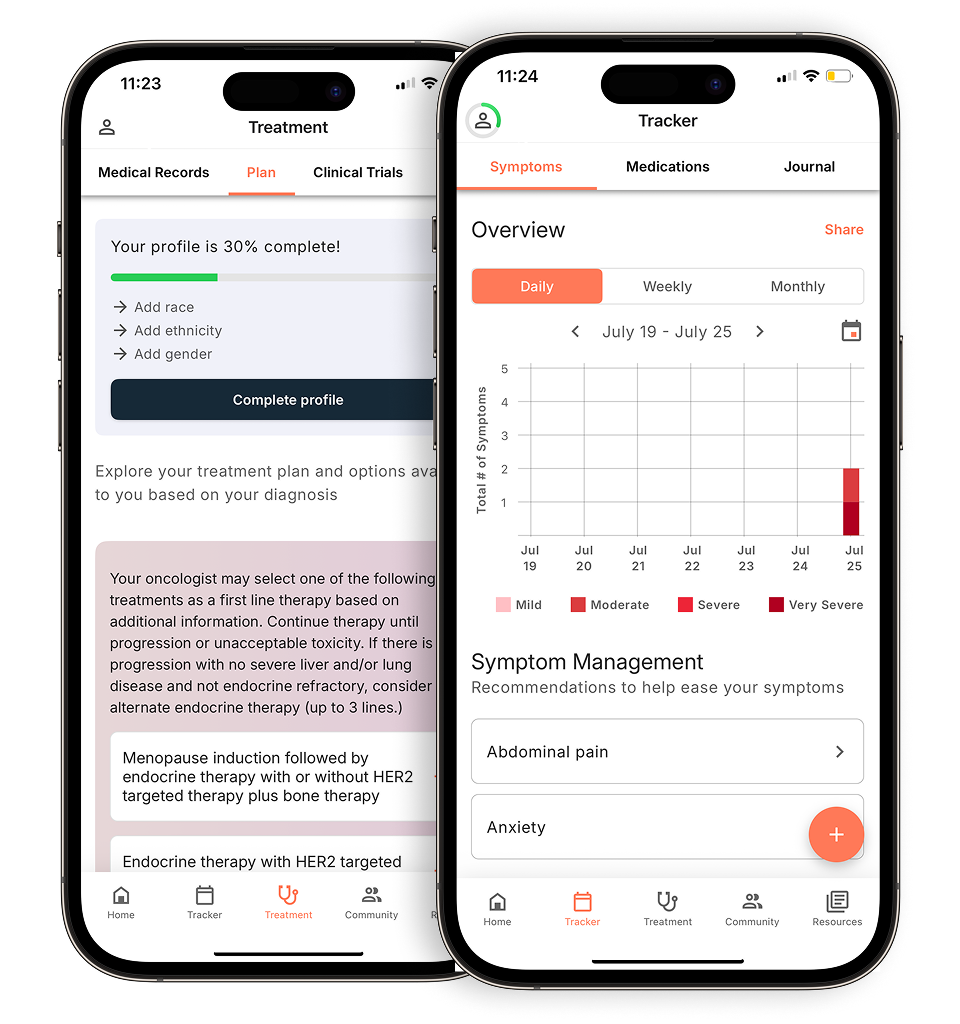
A: Sometimes we get the information we need, especially in a symptomatic patient, already from the bloodstream. A symptomatic patient typically has more tumor and more tumor means more tumor DNA in the bloodstream. The sensitivity of the liquid [e.g. blood] biopsy gets better. So, oftentimes, we get a histological diagnosis like an adenocarcinoma, but not enough tissue for a comprehensive molecular profile from the tissue. But, we can complement it with the information we get from the liquid biopsy. If a patient is not symptomatic or has very limited symptoms, oftentimes we recommend a re-biopsy. But in my experience, I think that’s shared by many of our colleagues, is that we are seeing incredibly strong sensitivity with the new NGS-based assays from the blood, so that in 80% of cases or so we’ll be able to make a genetic classification of the tumor based on the liquid biopsy alone. And, they still go together. But, oftentimes, we’re able to synthesize the information we have relatively quickly with the integration of the liquid biopsy.
Q: Do you ever have to start treatment before you have those molecular results? And when that happens, how does that play out for the patient?
A: I don’t see this much for non-small cell lung cancer. We do have empiric treatments for small cell lung cancer where the genetics are not quite as well understood, and small cell is even more of a medical emergency where patients need to get treated [quickly]. I really really try to avoid it [treating before results], and I haven’t had to in a long time, largely attributed to the availability of liquid biopsy. We always have the discussion with our patients…we really want to give every patient the best and most fitting and most effective treatment, and that requires having all the information pieces on the table. So patients [waiting to begin treatment] for an additional week can pay off in big ways. Later on, when we treat a patient with the appropriate therapy, you want to get to treatment fast, and we really try to avoid any unnecessary delays. We really try to get patients into the clinic within 48 hours and initiate our work-up steps very promptly, but I still would encourage to reserve [treatment until] the availability of genetic information in the context of decision-making. In 2024, liquid biopsy is so fast, it should be available, and especially in symptomatic patients, liquid biopsy sensitivity is excellent.
Q: Is it ever necessary to repeat biomarker testing whether immediately or during treatment?
A: The re-biopsy can be required sometimes if there’s a very little tumor shed. If there’s an earlier stage, the liquid biopsy may not be as sensitive in terms of genetic evolution. I think that’s very important. Once we start treating a cancer [it is] similar to when we treat a bacteria. Like with antibiotics, genetic adaptation, or genetic evolution, happens. So the initial genetic setup that we’re seeing is not the same that we’re seeing when a patient has been treated, so at every turn of events, every time a tumor starts acting differently, there has to be an explanation. Sometimes we don’t find the explanation, but we always try to. And so testing and retesting is very, very important. We have many patients now with EGFR lung cancer, for example, who have been tested three or four times as they go through the different lines of therapy, and it’s very important to not make the first, second, or third turn of decision-making uninformed. We really have to understand: what kind of cancer are we looking at at every time, at every turn of events? In particular, as we’re moving out, further clinical trial options and more nuanced decisions are coming into play, so I strongly recommend to stay on top of biopsies, liquid and tissue, and when the clinical behavior of a cancer changes and worsens.
To view the entirety of Dr. Dietrich’s Ask the Expert webinar, you can access it here.
Personalized support for real care decisions
Understand your diagnosis, explore clinical trials, and track symptoms--all in one place.
Get started
Compare treatments, prepare for appointments, and track side effects—all in the app
Built for your diagnosis, Outcomes4Me gives you the tools to make confident, informed decisions—right when you need them.
Continue in app