If you’ve been diagnosed with prostate cancer, you may have learned there’s a connection between hormones and the development of prostate cancer. To grow, prostate cancers need support from androgens, a group of hormones that are primarily responsible for biologically male attributes including testosterone and dihydrotestosterone.
One of the standard treatment paths for prostate cancer is hormone therapy, which works by suppressing your body’s production of testosterone. Keep reading to learn more about the different hormone therapy options.
How does hormone therapy work?
Hormone therapy helps treat prostate cancer by lowering androgen levels to cut off the supply of testosterone. This helps shrink and slow the growth of cancer. Although hormone therapy is often used to treat advanced prostate cancer, it can also be used to treat recurrent prostate cancer and early-stage prostate cancer with an intermediate/high risk of recurrence.
In a recent Outcomes4Me webinar with Dr. Xin Gao, a medical oncologist who practices at Massachusetts General Hospital, said, “Prostate cancer is pretty unique among cancers in that it really needs androgens and testosterone to grow, survive, spread, and we know that these medications can help in a variety of different ways.”
Why is hormone therapy used in metastatic prostate cancer?
In metastatic prostate cancer, the cancer has spread beyond the prostate to other areas of the body—such as the bones, distant lymph nodes, or other organs. Because the cancer is no longer confined to one place, removing the prostate won’t be enough to control the disease. That’s why hormone therapy, which works throughout the entire body, is used to slow the cancer wherever it has spread.
Hormone therapy doesn’t cure metastatic prostate cancer, but it can control it for many years, help relieve symptoms, and improve both survival and quality of life.
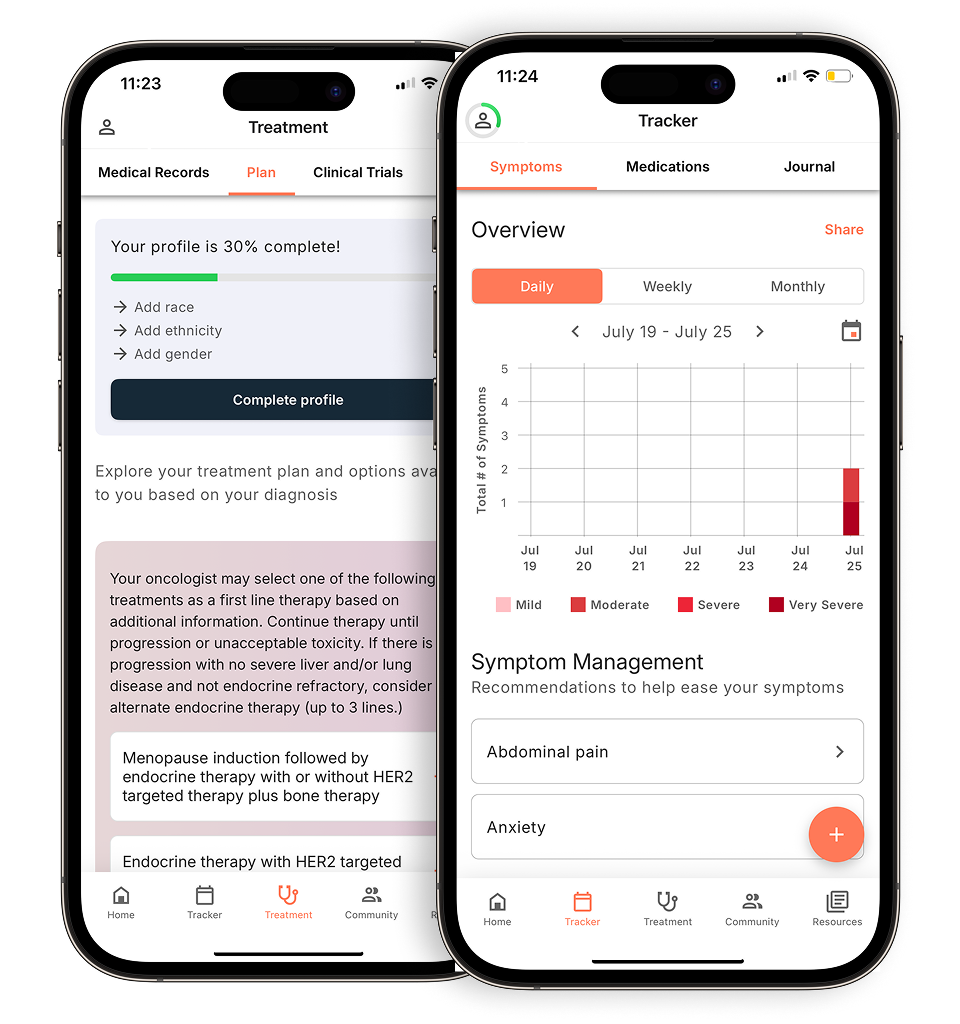
Evidence-based guidance powered by NCCN Guidelines®
Personalized treatment plans shaped by the latest oncology standards—tailored to your diagnosis.
Get started
View your personalized treatment plan in the Outcomes4Me app
Use your diagnosis to unlock personalized NCCN Guidelines®-aligned recommendations.
Continue in app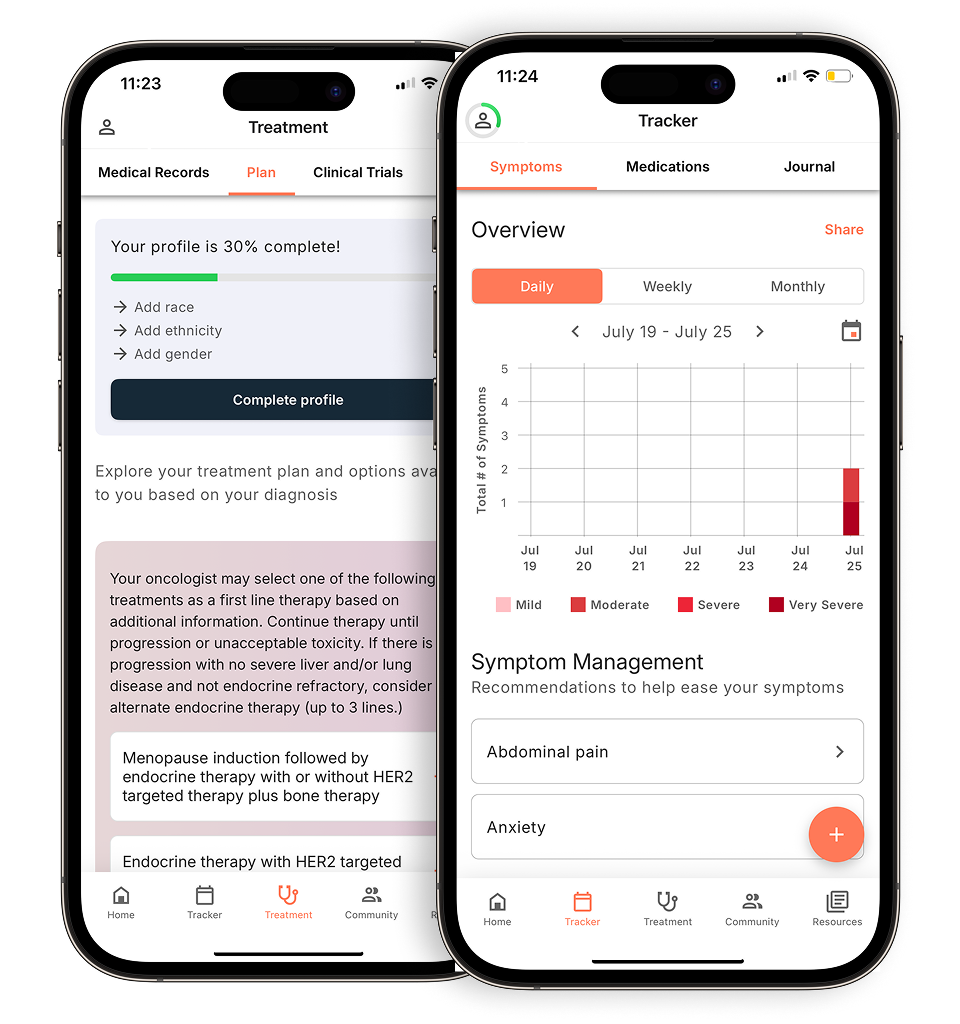
In some cases, your doctor may combine hormone therapy with other treatments—such as chemotherapy or newer advanced hormone blockers—to help you live longer and better. These combinations are often used when the cancer is growing quickly or involves many areas of the body.
How is hormone therapy given?
There are several ways your medical team may lower testosterone levels:
1) Injections or implants: Drugs like leuprolide (Lupron), goserelin (Zoladex), or triptorelin (Trelstar) are given every 1 to 6 months. These medications signal your body to stop making testosterone in the testicles. Some of these drugs initially cause a temporary testosterone flare, an increase in testosterone levels, before levels drop. Your doctor may prescribe a short-term medication to manage this.
2) Daily pills: Some medications such as relugolix (Orgovyx) also stop testosterone production and are taken by mouth each day. Unlike injections, they do not cause a hormone flare.
3) Surgery: Orchiectomy is a surgical procedure that removes the testicles to permanently lower testosterone. It’s fast, effective, and permanent but used less often today due to emotional and psychological concerns. Most men choose medication instead.
4) Anti-androgens: Sometimes, doctors prescribe another pill that works in a different way, such as bicalutamide (Casodex), enzalutamide (Xtandi), or apalutamide (Erleada), to block testosterone from reaching the cancer cells. This approach is called combined androgen blockade.
What to expect: common side effects
Because hormone therapy affects your whole body, it can cause side effects related to the loss of testosterone. Some men experience only mild changes, while others find the treatment more difficult. The most common side effects include:
- Hot flashes – Sudden waves of heat and sweating, similar to menopause in women
- Fatigue – Feeling unusually tired or low on energy
- Loss of interest in sex (low libido) or erectile dysfunction
- Mood changes – Irritability, sadness, or depression
- Weight gain, especially around the belly
- Loss of muscle or bone strength
Over time, hormone therapy may also impact your blood sugar, cholesterol, or heart health, so your care team may monitor these as well.
The good news is that many side effects can be managed. Let your care team know what you’re experiencing so they can help you stay comfortable and healthy.
How long is hormone therapy for prostate cancer?
The duration of hormone therapy depends on your individual cancer, treatment goals, and response to treatment. Some men stay on hormone therapy indefinitely, while others may use it in cycles (known as intermittent therapy) to give their body a break. Your doctor will regularly check your PSA level (a blood test that tracks prostate cancer activity) and testosterone level to guide treatment decisions.
Tips for managing life on hormone therapy
Living well with hormone therapy is possible. Here are some things you can do to help manage its effects:
- Stay active. Gentle exercise like walking, swimming, or light weight training can help fight fatigue, protect your bones and muscles, and lift your mood.
- Eat a healthy diet. Focus on lean proteins, vegetables, whole grains, and foods rich in calcium and vitamin D.
- Take care of your mind. Don’t ignore feelings of sadness, fear, or anxiety. Talking to a counselor or joining a support group can make a real difference.
- Protect your bones. Your doctor may give you a bone-strengthening medication like zoledronic acid (Zometa) or denosumab (Xgeva) if you’re at risk for fractures.
- Stay informed. Ask about your test results—especially PSA and testosterone levels—so you can track your progress and understand what they mean.
What if hormone therapy stops working?
Eventually, some prostate cancers may adapt and continue to grow even if you have very low testosterone levels. This is called castration-resistant prostate cancer (CRPC). When this happens, treatment doesn’t necessarily have to stop. Instead, your doctor may adjust your therapy using newer drugs that can still slow the disease.
It’s also important to remember that every individual might benefit from a different treatment plan, depending on their medical team’s assessment and the individual’s cancer profile.
According to Dr. Gao, “[Treatment options] come with different trade-offs; different logistical considerations. There are some patients who are truly a better fit for surgery rather than radiation-based therapies based on their specific factors and there are other patients who are actually better suited for radiation-based therapy than surgery.”
The bottom line
Hormone therapy is a key part of treating metastatic prostate cancer. It works by starving the cancer of testosterone, helping to slow it down and relieve symptoms. While it does come with side effects, many men live well for years on hormone therapy.
By learning what to expect and staying engaged with your care team, you can take an active role in your treatment. Ask questions, speak up about your symptoms, and remember that you are not alone on this journey.
If you have additional questions about hormone therapies or you’d like to speak with someone, you can connect with an Outcomes4Me oncology nurse practitioner at no charge through the Outcomes4Me app, using the “Ask Outcomes4Me” button.
Related Topics
- Understanding prostate cancer biomarker testing
- Therapy vs. surgery for prostate cancer
- Metastatic castration-resistant prostate cancer treatment options
- Advances in immunotherapy for prostate cancer treatment
- How precision medicine can help with prostate cancer
- What to know about robotic surgery for prostate cancer
Personalized support for real care decisions
Understand your diagnosis, explore clinical trials, and track symptoms--all in one place.
Get started
Compare treatments, prepare for appointments, and track side effects—all in the app
Built for your diagnosis, Outcomes4Me gives you the tools to make confident, informed decisions—right when you need them.
Continue in app