Adenocarcinoma, immunotherapy, biomarkers, chemoradiation—a new diagnosis can feel like learning a foreign language overnight. But you don’t have to be fluent to feel in control. We’re here to translate. This guide breaks down the core concepts, from adenocarcinoma non small cell lung cancer treatment to the latest therapies. We’ll explore the different advanced non small cell lung cancer treatment options, including the typical first line treatment for non small cell lung cancer, explaining how they work in simple terms. Our goal is to demystify the process so you can have more confident conversations with your healthcare team and choose the best path forward.
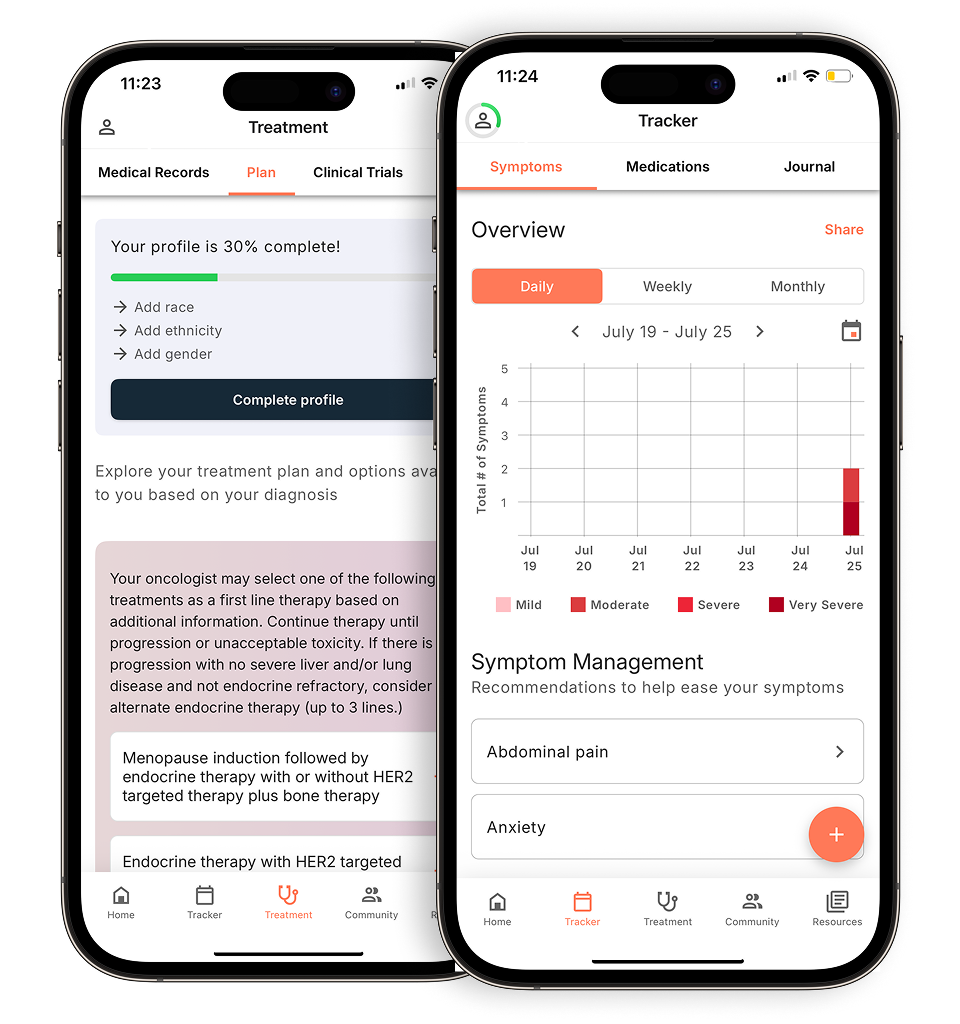
View your personalized treatment plan in the Outcomes4Me app
Use your diagnosis to unlock personalized NCCN Guidelines®-aligned recommendations.
Key Takeaways
- Your treatment plan is highly personalized: It’s designed around your cancer’s specific stage and genetic makeup, along with your overall health and personal goals.
- NSCLC is fought from multiple angles: Your care plan may combine different types of treatment, such as surgery for removal, radiation for local control, and systemic therapies like targeted drugs or immunotherapy to fight cancer throughout the body.
- You are the center of your care team: Ask questions, share your quality-of-life priorities, and use reliable resources to make informed decisions that align with your personal values.
What Is Non-Small Cell Lung Cancer (NSCLC)?
If you or a loved one has recently been diagnosed with lung cancer, you’ve likely heard the term “non-small cell lung cancer,” or NSCLC. It can feel overwhelming to learn a whole new vocabulary, but understanding the basics is the first step in feeling more in control. Simply put, non-small cell lung cancer is a type of cancer that forms in the tissues of the lungs. It’s the most common form of lung cancer, accounting for the vast majority of diagnoses.
Think of “lung cancer” as a broad category, with NSCLC being the largest group within it. The name comes from how the cancer cells look under a microscope. When doctors examine the cells, they see that they are larger than those found in the other main type of lung cancer. This distinction is more than just a name—it’s crucial because it helps your care team determine the best path forward for your treatment. Knowing you have NSCLC allows your oncologist to narrow down the most effective therapies and approaches for your specific situation.
How NSCLC Differs From Other Lung Cancers
The main distinction doctors make is between non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). While both start in the lungs, they behave very differently. SCLC is less common and is known for growing and spreading more quickly than NSCLC. Because of these differences in growth patterns, the treatment strategies for each type are quite distinct. Your diagnosis as having NSCLC means your treatment plan will be tailored to the specific characteristics of these larger cells, which often respond differently to therapies like surgery, targeted therapy, and immunotherapy compared to SCLC.
What Are the Main Types of NSCLC?
NSCLC isn’t just one disease; it’s a group of lung cancers. The main types are named for the kind of cells where the cancer begins and how they appear to a pathologist. Understanding which type you have is a key piece of the puzzle, as it can influence your treatment options.
The three primary types of NSCLC are:
- Adenocarcinoma: This is the most common type of NSCLC. It usually develops in the outer parts of the lungs and is often found in people who currently or used to smoke, but it’s also the most common type of lung cancer seen in non-smokers.
- Squamous Cell Carcinoma: This type typically starts in the flat, thin cells that line the airways in the central part of the lungs. It is very closely linked to a history of smoking.
- Large Cell Carcinoma: This is a less common type that can appear in any part of the lung. It tends to grow and spread quickly, which can make it more challenging to treat.
Common Symptoms of NSCLC
One of the challenging aspects of NSCLC is that it doesn’t always show clear signs in its early stages. Sometimes, there are no symptoms at all. When symptoms do appear, they can be mistaken for other, less serious conditions. It’s helpful to be aware of what to look for so you can have an informed conversation with your doctor. Common symptoms can include a cough that doesn’t go away or gets worse, chest pain, shortness of breath, wheezing, or coughing up blood. Some people also experience hoarseness, unexplained weight loss, or persistent fatigue. If any of these issues sound familiar, bringing them up with your healthcare provider is a proactive first step.
Causes and Risk Factors
When you hear “lung cancer,” your mind might immediately go to smoking. While that is a major piece of the puzzle, it’s not the whole story. A risk factor is anything that increases your chance of developing a disease, but it’s not a guarantee. Many people with risk factors never develop cancer, while others with no obvious risk factors do. Understanding the different factors that can contribute to NSCLC can provide a clearer picture of the disease and help you discuss your personal history with your care team. These factors range from lifestyle habits to environmental exposures and even your own family history.
The Role of Smoking and Secondhand Smoke
It’s true that smoking—whether cigarettes, cigars, or pipes—is the single biggest risk factor for developing NSCLC. The connection is direct: the longer a person smokes and the more they smoke, the higher their risk becomes. However, you don’t have to be the one smoking to be affected. Exposure to secondhand smoke also significantly increases the risk. This is because the same cancer-causing substances are present in the smoke that comes from the end of a cigarette and in the smoke exhaled by a smoker. Quitting smoking at any age can dramatically reduce your risk and is one of the most impactful steps you can take for your lung health.
Environmental and Genetic Risk Factors
Beyond smoking, several other factors can play a role in the development of NSCLC. Your environment and workplace can expose you to harmful substances, such as asbestos, certain chemicals, and air pollution. Another significant risk is radon, a naturally occurring radioactive gas that can get trapped in homes and buildings. Past radiation therapy to the chest for other cancers can also increase risk. Your personal and family history matters, too; having a close relative with lung cancer or a personal history of HIV infection can make you more susceptible. Finally, the risk of NSCLC increases with age, making it more common in older adults.
How NSCLC Is Diagnosed
The path to a diagnosis usually begins when you report symptoms to your doctor or when an imaging test for another issue reveals something unusual in your lungs. To get a better look, your doctor will likely start with imaging tests like a chest X-ray or a computed tomography (CT) scan. These scans create detailed pictures of your lungs and can show the location, size, and shape of any potential tumors. While these images are incredibly useful for identifying areas of concern, they can’t confirm whether a growth is cancerous on their own. They are the first step in a process that leads to more definitive testing.
Imaging Tests and Biopsies
If an initial scan shows a suspicious spot, the next essential step is a biopsy. A biopsy is a procedure where a small sample of tissue is removed from the suspicious area in the lung. A specialist called a pathologist then examines these cells under a microscope to determine if cancer is present. This is the only way to get a definite diagnosis. If cancer is confirmed, your doctor will order more tests to see if it has spread to other parts of your body. These can include a PET scan, an MRI, or a bone scan. The results of the biopsy and these follow-up scans provide the critical information your care team needs to determine the cancer’s stage and build a treatment plan tailored specifically to you.
Is Surgery an Option for NSCLC?
For many people diagnosed with non-small cell lung cancer (NSCLC), surgery is a key part of the treatment plan, especially when the cancer is caught early. The main goal of surgery is to completely remove the tumor along with a small margin of healthy tissue around it. This approach offers the best chance of a cure because it aims to eliminate the cancer before it has had a chance to spread to other parts of the body. Think of it as removing the problem at its source.
Deciding if surgery is the right path for you is a collaborative conversation you’ll have with your oncology team. They will look at several factors, including the specific type of NSCLC you have, the tumor’s size and location, and the cancer’s stage. Your overall health is also a major consideration. Your team needs to be confident that your heart and lungs are strong enough to handle both the procedure and the recovery process that follows. This ensures the benefits of the surgery outweigh the potential risks.
Ultimately, your treatment plan is tailored to you. Surgery might be the only treatment you need, or it could be combined with other therapies like chemotherapy or radiation to give you the best possible outcome. Your doctors will walk you through all the options, benefits, and risks, ensuring the final decision aligns with your health needs and personal preferences.
Are You a Candidate for NSCLC Surgery?
The best candidates for surgery are typically patients with early-stage NSCLC. This means the cancer is confined to one area of the lung and hasn’t spread to lymph nodes or distant organs. When the tumor can be completely removed, surgery offers the best chance for a cure. Your doctor will run a series of tests, including imaging scans and possibly a biopsy, to determine the exact stage of your cancer.
Beyond the cancer’s stage, your general health plays a crucial role. Your care team will evaluate your lung function to ensure you’ll be able to breathe well after a portion of your lung is removed. They’ll also consider any other health conditions you may have, like heart disease or diabetes, to make sure you’re physically prepared for the operation and recovery.
What Surgical Procedures Treat NSCLC?
Your surgeon will recommend a specific procedure based on the size and location of your tumor. The goal is always to remove all the cancer while preserving as much healthy lung tissue as possible. The most common surgical options include:
- Wedge resection: Removes a small, wedge-shaped piece of the lung that contains the tumor.
- Lobectomy: Removes an entire section, or lobe, of the lung. This is one of the most common surgeries for NSCLC.
- Pneumonectomy: Removes the entire lung on one side. This is reserved for cases where the tumor is large or centrally located.
- Sleeve resection: Removes a piece of the main airway (bronchus) and then reattaches the ends.
Your doctor will explain which of these surgical options is most appropriate for your situation.
Your Surgical Recovery: What to Expect
Recovering from lung surgery takes time, and it’s important to be patient with yourself. You can expect to feel some pain, fatigue, and shortness of breath in the beginning, but your healthcare team will be there to help you manage these symptoms. They will provide pain medication and guide you through breathing exercises and a gradual return to activity to help you regain your strength.
In some cases, your doctor may recommend additional treatments after surgery, such as chemotherapy or targeted therapy. This is known as adjuvant therapy, and its purpose is to destroy any cancer cells that might have been left behind, reducing the chance of the cancer returning. Following your care team’s advice for recovery and rehabilitation is the best way to ensure a smooth and successful healing process.
Other Localized Treatments for NSCLC
While surgery is a common and effective approach, it’s not the only way to treat non-small cell lung cancer that is confined to one area. For some people, surgery might not be the best option due to other health concerns or the specific location of the tumor. In these cases, your care team has other powerful tools that can target the cancer directly. These localized treatments are designed to destroy cancer cells with incredible precision, often with less impact on the rest of your body. They can be used on their own or sometimes in combination with other therapies to create a comprehensive plan that’s tailored just for you.
Stereotactic Body Radiation Therapy (SBRT)
Think of Stereotactic body radiation therapy, or SBRT, as a highly advanced form of radiation. Instead of treating a wide area, SBRT uses sophisticated technology to deliver very high doses of radiation directly to the tumor in just a few sessions. This technique is incredibly precise, allowing your doctors to target the cancer cells while minimizing exposure and damage to the healthy tissues surrounding them. It’s a particularly valuable option for patients with early-stage, localized tumors who may not be candidates for surgery due to other health conditions. SBRT offers a non-invasive way to effectively control the cancer with a shorter treatment course than traditional radiation.
Other Therapies for Airway Tumors
Sometimes, a tumor can grow in a way that blocks one of the main airways in your lungs, which can make breathing difficult. When this happens, your doctor may recommend a specialized procedure to clear the blockage and relieve your symptoms. These treatments are performed using a bronchoscope—a thin, flexible tube that is guided down your throat and into the airways. This approach allows your doctor to directly access and treat the tumor without making any incisions. It’s a targeted way to address a specific problem and can make a significant difference in your comfort and quality of life.
Laser Therapy and Photodynamic Therapy (PDT)
Two common methods for treating airway tumors are laser therapy and photodynamic therapy (PDT). With laser therapy, your doctor uses a high-energy beam of light to destroy cancer cells and remove the part of the tumor that is causing the obstruction. It’s a quick and effective way to reopen the airway. Photodynamic therapy is a two-step process. First, you’re given a light-sensitive drug that is absorbed by cells throughout your body. This drug leaves healthy cells quickly but stays in cancer cells longer. A day or two later, your doctor uses a special light to activate the drug specifically in the tumor, which then destroys the cancer cells.
Cryosurgery and Electrocautery
Cryosurgery and electrocautery are two other techniques that can be used to treat tumors in the airways. They work in opposite ways but achieve a similar goal. Cryosurgery uses extreme cold to freeze and destroy the abnormal tissue. Your doctor applies liquid nitrogen or argon gas directly to the tumor, causing the cancer cells to die. On the other hand, electrocautery uses heat. An electric current is passed through a small probe to burn away the cancerous tissue. Both of these methods are effective for treating localized tumors and can be performed through a bronchoscope to help clear your airways and improve your breathing.
Chemotherapy and Radiation: How Do They Work?
When you’re building a treatment plan for non-small cell lung cancer (NSCLC), chemotherapy and radiation therapy are two of the most established and effective tools your oncology team might recommend. These treatments work in different ways to attack cancer cells, and they can be used alone or together, depending on your specific diagnosis and cancer stage. Think of them as a powerful one-two punch against cancer. Understanding how they function can help you feel more prepared and confident as you begin treatment. Let’s walk through what each one does and what it means to use them in combination.
How Chemotherapy Fights NSCLC
Chemotherapy, often called “chemo,” uses powerful drugs to destroy cancer cells or stop them from multiplying. Because cancer cells tend to grow and divide very quickly, they are especially vulnerable to these drugs. The medication typically travels through your bloodstream, allowing it to reach cancer cells throughout your body. This makes it a systemic treatment, meaning it can fight cancer that may have spread from the original tumor. Your care team may use a single drug or a combination of drugs, such as carboplatin, cisplatin, and paclitaxel, to create the most effective NSCLC treatment plan for you.
What Are the Types of Radiation Therapy?
Radiation therapy uses high-energy rays, like X-rays, to damage cancer cells and stop them from growing. Unlike chemo, radiation is a local treatment, which means it targets a specific area of your body. There are two main types of radiation therapy for NSCLC. The most common is external beam radiation, where a machine outside your body aims beams of radiation directly at the tumor. Another type is internal radiation, or brachytherapy, where a radioactive source is placed inside your body, either in or near the cancer. Your radiation oncologist will determine the best approach based on the tumor’s size and location.
Combining Chemo and Radiation: What to Know
Sometimes, the most effective strategy is to use chemotherapy and radiation at the same time, a practice known as concurrent chemoradiation. The chemotherapy can make cancer cells more sensitive to the radiation, which can make the combined treatment more powerful than using either one on its own. While this approach can be very effective, it can also lead to more intense side effects. It’s common to experience fatigue, skin reactions at the radiation site, digestive issues, and hair loss. Your care team is there to help you manage side effects and will work closely with you to keep you as comfortable as possible.
Targeted Therapy: A Precision Lung Cancer Treatment Option
Imagine a treatment that’s less like a broad-spectrum attack and more like a key designed for a specific lock on cancer cells. That’s the idea behind targeted therapy. Unlike chemotherapy, these drugs are designed to zero in on the specific characteristics that help cancer cells grow and survive. This precision approach uses your tumor’s unique genetic fingerprint to fight the cancer more effectively, often with fewer of the side effects associated with traditional treatments.
Why Genetic Testing and Biomarkers Matter
Before starting targeted therapy, your oncology team will recommend biomarker testing on a sample of your tumor. This testing looks for specific genetic changes, or mutations, that drive the cancer’s growth. Think of these as the cancer’s Achilles’ heel. For NSCLC, common mutations include changes in genes like EGFR, ALK, and ROS1. Finding one of these biomarkers means there may be a targeted drug specifically designed to attack that weakness. This is why genetic testing is such a critical step in creating a personalized treatment plan that gives you the best chance for success.
Biomarker Testing for PD-L1, KRAS, and More
While EGFR, ALK, and ROS1 are some of the most well-known biomarkers, the list of important genetic targets is constantly expanding. Your oncologist will likely test for a broad panel of mutations to get the fullest picture of your cancer. This includes looking for biomarkers like KRAS, one of the most common mutations in NSCLC, especially in people with a history of smoking. For years, KRAS was notoriously difficult to target, but recent breakthroughs have led to new drugs for specific KRAS mutations. Another key biomarker is PD-L1, a protein that helps cancer cells evade the immune system. High levels of PD-L1 can indicate that you might be a good candidate for immunotherapy, a treatment that helps your own immune system fight the cancer.
Patient Factors That Correlate with Certain Mutations
Researchers have found that certain genetic mutations appear more often in specific groups of people. For example, EGFR gene mutations are more frequently seen in women, non-smokers, people of Asian descent, and those with the adenocarcinoma subtype of NSCLC. It’s important to remember that these are just statistical trends, not hard-and-fast rules. Anyone can have any type of mutation, which is why comprehensive biomarker testing is so vital for every single person diagnosed with NSCLC. These patterns simply help researchers understand the disease better, but they don’t replace the need for personalized testing to guide your unique treatment plan.
What Targeted Therapy Drugs Are Used for NSCLC?
Once your biomarker test results are in, your doctor can match you with the right medication. There are many targeted therapy drugs available, and new ones are approved regularly. For example, if your cancer has an EGFR mutation, your doctor might discuss drugs like afatinib or erlotinib. If an ALK mutation is found, a drug like crizotinib might be an option. These are just a few examples, and the specific drug recommended for you will depend entirely on your tumor’s unique genetic profile. These medications are typically pills you can take at home, making treatment more convenient than IV infusions.
Drugs for EGFR Mutations
If your tumor has an EGFR mutation, your doctor may recommend a class of drugs called EGFR inhibitors. These medications are designed to block the signals that tell cancer cells to grow and divide. For patients with this specific mutation, these drugs can be much more effective than traditional chemotherapy. Studies have shown that treatments like gefitinib and erlotinib can keep the cancer under control for significantly longer and are more likely to shrink tumors. This is a perfect example of how knowing your tumor’s genetic makeup can directly lead to a more effective, personalized treatment that is tailored just for you.
Drugs for KRAS, ROS1, MET, and RET Mutations
EGFR is just one of several important biomarkers in NSCLC. Genetic testing can reveal other mutations that also have specific targeted drugs designed to fight them. For instance, a KRAS G12C mutation can be treated with sotorasib, often after other therapies have been tried. If your cancer is ROS1-positive, drugs like crizotinib or entrectinib may be options. For MET exon 14 skipping mutations, your doctor might suggest tepotinib or capmatinib, especially if surgery isn’t possible. Similarly, a RET-positive cancer can be treated with pralsetinib. Each discovery of a new biomarker opens up another avenue for precision treatment, making comprehensive testing a vital part of your care.
Targeted Therapy: Benefits vs. Side Effects
A major advantage of targeted therapy is that it often has a different side effect profile than chemotherapy. Because these drugs are more precise, they tend to cause less damage to healthy cells. However, they are not without side effects. Common issues can include skin rashes, diarrhea, and changes in liver function. It’s important to talk with your healthcare team about what to expect and how to manage side effects. They can provide strategies and medications to help you feel your best throughout your treatment, ensuring your quality of life remains a top priority.
How Does Immunotherapy Treat NSCLC?
Immunotherapy is a powerful approach that works differently from chemotherapy or radiation. Instead of directly attacking cancer cells with outside agents, this NSCLC treatment helps your body’s own immune system recognize and fight the cancer. Think of it as training your internal defense team to identify and target cancer cells that were previously able to hide.
This type of therapy can be a game-changer in how we approach lung cancer. Depending on your specific situation, your doctor might recommend immunotherapy at different points in your treatment journey. It can be given before surgery to help shrink a tumor, after surgery to eliminate any remaining cancer cells, or sometimes in combination with other treatments like chemotherapy to create a multi-pronged attack against the cancer. The goal is always the same: to use the natural power of your body to control the disease.
How Your Immune System Can Fight Cancer
So, how does immunotherapy actually work? Your immune system is designed to find and destroy foreign invaders like bacteria and viruses. However, cancer cells can be tricky. They often develop ways to disguise themselves, essentially putting up a “don’t attack me” signal to your immune cells. Immunotherapy drugs are designed to interfere with these signals.
These medications work by blocking the proteins that cancer cells use to hide. By doing this, they effectively take the blinders off your immune cells, allowing them to see the cancer for what it is and get to work. These drugs help your T-cells—a key part of your immune response—find and kill cancer cells more effectively, turning your own body into a more powerful ally in your fight.
What Are the Types of Immunotherapy Drugs?
There are several immunotherapy drugs approved to treat non-small cell lung cancer, and they often fall into a category called “immune checkpoint inhibitors.” While you don’t need to memorize every name, you might hear your oncologist mention drugs like atezolizumab (Tecentriq), nivolumab (Opdivo), or pembrolizumab (Keytruda). Each of these works to block specific checkpoint proteins, such as PD-1, PD-L1, or CTLA-4, which are the “hiding” signals cancer cells use. Your medical team will determine the most appropriate drug or combination for your specific type of NSCLC based on its unique characteristics.
Is Immunotherapy a Good Fit for You?
Immunotherapy isn’t the right choice for every person with NSCLC, and several factors go into making that decision. Your treatment choices will depend heavily on how far the cancer has spread, which is known as its stage. Your overall health and how well your lungs are functioning also play a significant role in determining if your body can handle this type of treatment.
Beyond that, specific features of the cancer itself are critical. Your doctor will likely test your tumor for certain biomarkers, like the level of the PD-L1 protein. A higher level of PD-L1 can sometimes indicate that immunotherapy will be more effective. This is why personalized testing is so important—it helps your care team match you with the treatment that has the best chance of success.
How Does Cancer Stage Affect Your Treatment?
Think of your cancer’s stage as a map that shows your care team exactly where the cancer is, how large it is, and whether it has spread. This information is one of the most important factors in building your treatment plan. The stage helps determine the primary goal of your treatment, which can range from aiming for a complete cure to focusing on controlling the cancer’s growth and managing symptoms to preserve your quality of life.
For early-stage cancers that are confined to one area, the treatment strategy is often more aggressive, with the goal of removing or destroying all cancer cells. As the cancer becomes more advanced and spreads, the approach may shift. Treatment becomes more about managing the disease as a chronic condition, using systemic therapies that travel throughout the body to fight cancer cells wherever they are. Your oncologist will use the stage, along with other factors like your overall health and the cancer’s genetic makeup, to recommend a path forward that’s right for you. Below, we’ll explore how treatment approaches typically differ for early, advanced, and metastatic NSCLC.
Your Treatment Options for Early-Stage NSCLC
When NSCLC is caught early (like Stage 0 or I), the tumor is typically small and hasn’t spread beyond the lungs. In these cases, the main goal is often a cure. Surgery to remove the tumor is usually the first and most important step. For many people with Stage I NSCLC, a procedure called a lobectomy, which removes an entire lobe of the lung, offers the best chance for a cure and may be the only treatment needed. After surgery, your doctor might recommend additional treatments like chemotherapy, targeted therapy, or immunotherapy if there’s a high risk the cancer could return. This is called adjuvant therapy, and it acts as an extra layer of security.
Defining Occult, Stage 0, Stage I, and Stage II
Let’s break down what these earliest stages mean, as this is where treatment is often most straightforward. Occult cancer is a unique situation where cancer cells are found, for example in a sample of phlegm, but doctors can’t yet see a tumor on imaging scans. The typical approach here is close monitoring until a tumor becomes visible, at which point a treatment plan can begin. Stage 0 is the earliest possible stage. Here, the cancer is confined to the very top lining of the airways and hasn’t spread any deeper. Because it’s so contained, it’s often curable with surgery alone, though sometimes other localized treatments like laser therapy are used instead.
In Stage I, a tumor is present but is still contained within the lung and hasn’t reached any lymph nodes. Surgery is the primary treatment and is often all that’s needed to offer a cure. For Stage II, the cancer is a bit more advanced—the tumor may be larger, or it may have spread to nearby lymph nodes. The treatment plan for Stage II often involves more steps, potentially including chemotherapy or immunotherapy before surgery to shrink the tumor, followed by the operation and possibly more treatment afterward to address any remaining cancer cells.
Advanced Non-Small Cell Lung Cancer Treatment Options
If your cancer is more advanced but still contained within the chest (often Stage III), your treatment plan will likely involve a combination of therapies. Because the tumor may be too large or in a difficult spot for surgery alone, doctors often use a powerful one-two punch of chemotherapy and radiation, known as chemoradiation. Your overall health plays a big role here, as combination treatments can be demanding. If you aren’t healthy enough for this approach, your doctor might suggest radiation or chemotherapy on its own. Immunotherapy is also becoming a common first-line treatment option for advanced-stage NSCLC, sometimes used alongside chemotherapy.
Defining Stage III
Stage III NSCLC means the cancer has grown more extensive within the chest but hasn’t spread to distant parts of the body. Because the tumor might be larger or located near important structures, surgery alone often isn’t enough. Instead, your care team will likely recommend a combination of treatments to attack the cancer from multiple angles. A common and powerful approach is chemoradiation, where you receive both chemotherapy and radiation therapy. The goal is for the chemo to weaken cancer cells throughout the chest, making them more vulnerable to the targeted high-energy beams of radiation. Your overall health is a key factor in this decision, as this combined therapy can be tough on the body. If it’s too demanding, your doctor may suggest using just one of these treatments to align with your specific cancer stage and health status.
Specific Immunotherapy Strategies for Stage III
After completing chemoradiation, your treatment journey for Stage III NSCLC may not be over. This is often when immunotherapy steps in. Your doctor might recommend a type of immunotherapy called an immune checkpoint inhibitor as a follow-up treatment. The goal here is to empower your own immune system to do a “clean-up” mission, seeking out and destroying any stubborn cancer cells that may have survived the initial treatment. This approach has been shown to help keep the cancer from returning for a longer period. In some situations, immunotherapy might even be used alongside chemotherapy *before* surgery to help shrink the tumor, making it easier to remove. This highlights how personalized your treatment plan is, adapting to your specific cancer and health needs.
How Is Metastatic NSCLC Treated?
Metastatic, or Stage IV, NSCLC means the cancer has spread to other parts of the body, like the brain, bones, or liver. At this stage, the cancer is very difficult to cure. The primary goal of treatment shifts to helping you live longer and feel better by controlling the cancer’s growth and managing symptoms. Your treatment plan will be highly personalized, often involving a mix of chemotherapy, targeted therapy, immunotherapy, and radiation. Because this is an area of active research, participating in clinical trials can be an excellent option, giving you access to new and promising treatments. In some cases, if the cancer has only spread to one other location, your doctor may recommend more aggressive treatment like surgery or radiation to that specific spot.
Defining Stage IV (IVA and IVB)
When NSCLC is classified as Stage IV, it means the cancer has metastasized, or spread, from the lungs to other parts of the body. This might include distant lymph nodes, the brain, bones, or liver. At this point, the focus of your treatment will likely shift. While a cure is very difficult to achieve, the primary goal becomes controlling the cancer’s growth and managing your symptoms to help you live longer and maintain the best possible quality of life. Your care plan will be highly unique to you, often combining systemic treatments like targeted therapy, immunotherapy, or chemotherapy. Because this is an area where cancer research is rapidly advancing, your doctor may also talk to you about clinical trials, which can provide access to the latest, most promising therapies.
Treating Recurrent or Progressive NSCLC
It can be disheartening to learn that your cancer has returned after treatment (recurrent) or has continued to grow during treatment (progressive). But it’s important to know that this doesn’t mean the end of the road. Your oncology team will re-evaluate your situation to decide on the next steps. This decision depends on several factors, including where the cancer is now, which treatments you’ve already had, and your overall health. The goal of this next phase of further treatment could be to slow the cancer’s growth or to relieve symptoms and keep you comfortable. Your options might include another round of chemotherapy, different targeted therapies, immunotherapy, or localized treatments like radiation to manage specific spots.
Understanding Second-Line Treatments
When your first treatment plan stops being effective, your doctor may recommend a “second-line treatment.” This is a standard approach for patients who are still feeling relatively well and are ready to continue fighting the cancer. The goal is to find a different therapy that the cancer will respond to. For example, studies have shown that second-line drugs like docetaxel or erlotinib can significantly slow cancer growth and help people live longer compared to receiving only supportive care. This approach is all about extending your time and ensuring you feel as good as possible, giving you more options and more hope as you continue your journey.
What Factors Guide Your Treatment Plan?
Creating a treatment plan for non-small cell lung cancer is a deeply personal process. There is no single “best” path; instead, your oncologist will work with you to develop a strategy that considers your unique situation. The right approach for you will depend on a combination of your health, the specific characteristics of the cancer, and your own personal priorities. Together, you and your care team will weigh these factors to make informed decisions every step of the way.
How Does Your Health Affect Treatment Choices?
Before recommending a course of action, your doctor will consider your general health. Are you managing other health conditions? How strong is your body right now? These aspects influence which treatments you can tolerate. Specifically for lung cancer, your lung function is a critical piece of the puzzle. Some treatments, particularly surgery, require healthy enough lungs to handle the procedure and recovery. Your team will choose NSCLC treatment options that are both effective and safe for your specific health profile.
Why Your Tumor’s Genetics Are Important
Modern cancer care goes beyond the microscope to look at the tumor’s genetic makeup. Your doctor may recommend biomarker testing to identify specific gene changes (mutations) in the cancer cells that help them grow. Finding these markers can open the door to targeted therapy, a type of treatment that uses drugs to attack those specific changes. For example, some therapies work best for cancers with mutations in genes like EGFR or ALK. This precision approach allows for a more personalized and effective treatment plan.
How Histology (Squamous vs. Non-Squamous) Impacts Treatment
Beyond genetics, the specific type of cell your cancer started in—its histology—is another critical piece of the puzzle. The main distinction is between squamous and non-squamous NSCLC (which includes adenocarcinoma and large cell carcinoma). This isn’t just a technical detail; it directly guides which chemotherapy drugs your oncologist will recommend. For example, patients with non-squamous tumors may benefit from drugs like pemetrexed or bevacizumab, which are often not used for squamous cell cancers due to a lack of effectiveness or potential for serious side effects. Knowing your cancer’s histology ensures your treatment is not only tailored to your tumor’s genetic profile but also to its fundamental cell type, giving you the safest and most effective path forward.
Aligning Treatment with Your Personal Goals
Your voice is one of the most important factors in this process. Making decisions about your treatment is a personal journey, and your goals and priorities matter immensely. What does quality of life mean to you? Are you hoping to manage symptoms, maintain your independence, or pursue an aggressive treatment? It’s essential to have open conversations with your care team and loved ones about what you hope to achieve. This allows you to work closely with your doctors to choose a path that aligns with your values, balancing the benefits of a treatment with its possible side effects.
What to Expect From Your Treatment
Starting treatment can bring up a lot of questions about what lies ahead. While every person’s experience is unique, understanding the basics of managing side effects, separating fact from fiction, and knowing your care options can help you feel more prepared. Your treatment journey is about more than just fighting cancer; it’s also about maintaining your quality of life every step of the way. Open communication with your care team is key, as they are your best resource for handling any challenges that arise.
How to Manage Treatment Side Effects
Most cancer treatments come with side effects, but you don’t have to simply endure them. Your first and most important step is to talk with your healthcare team about any symptoms you experience. They can offer medications, adjust your treatment, or refer you to specialists. You can also ask about palliative care, which is specialized medical care focused on providing relief from the symptoms and stress of a serious illness.
Simple, at-home strategies can also make a big difference. Gentle breathing exercises or progressive muscle relaxation can help manage stress. For nausea, try sucking on ice chips and avoiding lying down right after eating. Staying hydrated by drinking plenty of water is also crucial for managing many common side effects.
Debunking Common Myths About NSCLC Treatment
Misinformation about lung cancer can create unnecessary fear and confusion. One of the most persistent lung cancer misconceptions is that it’s only a disease that affects people who smoke. The truth is, anyone can get lung cancer, regardless of their history with tobacco.
Another common myth is that older patients are too frail for effective treatment. This is simply not true. Age alone doesn’t determine your ability to tolerate therapy. Inaccurate assumptions about treatment tolerance can unfortunately lead to less effective care. Your overall health, lung function, and personal preferences are far more important factors in creating a treatment plan that’s right for you.
Why Supportive Care Is a Key Part of Treatment
Supportive care is a critical part of your cancer treatment that focuses on your comfort and quality of life. It’s designed to help you manage symptoms, side effects, and the emotional stress that can come with a cancer diagnosis. It’s important to know that supportive care is not just for end-of-life situations; it can and should be integrated from the very beginning of your treatment.
Even if your cancer is not curable, it is still treatable. Treatment can often extend life and improve your day-to-day well-being. And remember, supportive care is always an option. Even if you decide to stop active cancer treatment, you can continue to receive care that helps with pain, breathing difficulties, and other symptoms.
The Importance of Quitting Smoking for Better Outcomes
It’s a well-known fact that smoking is the biggest risk factor for lung cancer, but let’s focus on the present: if you currently smoke, quitting is one of the most powerful actions you can take for your health. This isn’t about looking back; it’s about moving forward. Research consistently shows that patients who stop smoking after a lung cancer diagnosis have better results. Quitting can actually improve how effective your treatment is and can lead to better overall survival rates. It’s also important to avoid secondhand smoke, as exposure can also affect your health. Your care team can connect you with resources to help you quit, giving you another tool to actively participate in your own care and work toward the best possible outcome.
How to Get Personalized Treatment Guidance
Figuring out your NSCLC treatment options can feel like a lot to handle, but you don’t have to do it alone. The goal is to create a personalized plan that fits your specific diagnosis, health, and life goals. This isn’t about finding a one-size-fits-all answer, but about creating a path forward that feels right for you. Getting this kind of tailored guidance involves a few key steps: working closely with your medical experts, knowing what to ask, and using reliable tools to stay informed.
Think of it as assembling your personal support system. Your healthcare providers bring the medical expertise, you bring the knowledge of your own body and priorities, and digital resources can help bridge the gap. By combining these elements, you can feel more confident and in control of your treatment decisions. It’s all about collaboration and clear communication. Let’s walk through how you can actively participate in shaping your care plan.
How to Partner with Your Healthcare Team
You’ll have a dedicated group of experts, often called a Multidisciplinary Team (MDT), working together to map out your treatment. This team isn’t just one doctor; it typically includes oncologists, surgeons, nurses, and other specialists who all bring their unique perspectives to the table. Their goal is to collaborate and create a comprehensive care plan tailored specifically to you. This team approach ensures that all aspects of your health are considered, from the specifics of your cancer to your overall well-being. You are the central member of this team, and their collective expertise is one of your greatest resources.
Key Questions to Ask Your Oncologist
Your appointments are the perfect time to get clarity and voice your thoughts. To make the most of these conversations, it helps to come prepared. Think about what matters most to you, whether it’s maintaining a certain quality of life or understanding all potential outcomes. Be sure to discuss the benefits of each treatment option alongside the possible risks and side effects. A great starting point is asking, “What are all of my treatment options?” followed by, “How will each one impact my daily life?” Don’t hesitate to bring a family member or friend to help you listen and take notes. Your cancer care team is there to help you understand everything.
Finding Trusted Guidance with Digital Tools
Beyond your direct medical team, digital tools can provide an extra layer of support and information. These resources can help you make sense of your diagnosis, learn about treatment options, and even find relevant clinical trials. Your doctor might suggest a clinical trial, which are studies that test new and potentially better ways to treat cancer. Participating in one can give you access to cutting-edge care while contributing to medical progress. Apps like Outcomes4Me can help you securely organize your medical records and receive personalized guidance based on the latest evidence-based guidelines, making it easier to have informed discussions with your doctor.
What’s Next? Clinical Trials and New Treatments
The world of cancer care is always moving forward. Researchers and doctors are constantly working to find newer, better ways to treat non-small cell lung cancer. This dedication means that the treatment landscape today looks very different than it did even a few years ago, with more effective and often gentler options available. For patients, this progress offers real hope.
Two of the most exciting areas of progress are clinical trials and the development of new therapies. Clinical trials are research studies that give patients access to cutting-edge treatments before they are widely available. They are the engine that drives every medical breakthrough. At the same time, recent advancements like targeted therapies and immunotherapies are already changing what it means to live with NSCLC. These treatments are more precise and personalized, marking a significant shift away from one-size-fits-all approaches. Staying informed about these developments is a powerful way to be an active partner in your own care.
How to Find and Join a Clinical Trial
A clinical trial is a research study that explores new treatments, new combinations of existing treatments, or new ways to use them. It’s a common misconception that trials are only a last resort; in reality, there are trials available for people with NSCLC at all stages. Participating can give you access to the next wave of therapies while contributing to medical science.
The best place to start is by talking with your oncologist. They can help you understand if a clinical trial is a good option for you and identify studies that match your specific diagnosis and health profile. You can also find clinical trials through trusted online databases from organizations like the National Cancer Institute.
Exploring the Latest Advances in NSCLC Treatment
Some of the most significant breakthroughs in NSCLC care have come from targeted therapies and immunotherapies. Unlike traditional chemotherapy, which affects all fast-growing cells, these treatments are much more precise. Targeted therapies work by identifying and attacking cancer cells with specific genetic mutations, while immunotherapies help your own immune system recognize and fight the cancer.
These advancements in NSCLC treatment are not only effective but can also improve quality of life. Many of these newer drugs are taken as pills at home and often come with fewer and less severe side effects than chemotherapy, allowing you to maintain more of your normal routine during treatment.
What Does the Future Hold for NSCLC Care?
The future of NSCLC care is incredibly promising. The research happening today is focused on creating even more personalized and effective treatments. Scientists are working to identify new biomarkers, develop smarter drugs, and find new ways to combine therapies for better results. Every clinical trial brings the medical community one step closer to turning NSCLC into a manageable condition.
Your doctor may talk to you about joining a study, as these are a key part of finding better ways to treat cancer. By staying engaged and asking questions about new treatment options for NSCLC, you place yourself at the forefront of care and contribute to a future where everyone affected by this disease has a better outcome.
Related Articles
- What are my options when lung cancer spreads and radiation stops working? | Outcomes4Me Community
- What new lung cancer treatments are available today? | Outcomes4Me Community
- What are the best pill treatment options for NTRK1 lung cancer after surgery? | Outcomes4Me Community
- What to expect after a small-cell lung cancer diagnosis – Outcomes4Me
- Small Cell Lung Cancer Survival Rates: Prognosis & Life Expectancy
View your personalized treatment plan in the Outcomes4Me app
Use your diagnosis to unlock personalized NCCN Guidelines®-aligned recommendations.
Frequently Asked Questions
Why is biomarker testing so important for my treatment plan? Think of biomarker testing as creating a detailed profile of your specific cancer. This testing looks for unique genetic changes in the tumor cells that help them grow. Finding these markers can open the door to highly specific treatments, like targeted therapy, which are designed to attack that exact weakness. It’s a crucial step that helps your care team move beyond a one-size-fits-all approach and choose a therapy that has the best chance of working for you.
What’s the real difference between targeted therapy and immunotherapy? It’s easy to get these two mixed up, but they work in very different ways. Targeted therapy uses drugs that act like a key fitting into a specific lock on the cancer cells, interfering with their ability to grow. Immunotherapy, on the other hand, doesn’t attack the cancer directly. Instead, it works by helping your own immune system recognize and destroy cancer cells that were previously able to hide from it.
If my cancer is advanced, what is the goal of treatment? When NSCLC has spread, the primary goal of treatment often shifts from a complete cure to controlling the cancer’s growth and managing your symptoms. The aim is to help you live longer and maintain the best possible quality of life. Your treatment plan will be highly personalized, often using a combination of therapies to manage the cancer much like a chronic condition, allowing you to feel better and stay active.
I’m worried about treatment side effects. What can I do about them? Feeling concerned about side effects is completely normal, but you don’t have to just push through them. Managing side effects is a key part of your overall treatment plan. The most important thing you can do is communicate openly with your care team about how you’re feeling. They can offer medications, suggest lifestyle adjustments, or connect you with supportive care specialists who focus entirely on helping you manage symptoms and feel more comfortable from day one.
Is surgery always the main treatment for early-stage lung cancer? Surgery is a very common and effective treatment for early-stage NSCLC, as it offers the best chance to remove the cancer completely. However, it isn’t the right choice for everyone. Your oncology team will consider many factors, including the exact size and location of the tumor and, just as importantly, your overall health and lung function. The final decision is a collaborative one made with you to ensure the chosen path is both safe and effective for your situation.